History
A 67 year old male was referred to us for palliative management of right-sided pleural mesothelioma with thoracic and abdominal metastases. Other than a history of hypertension, the patient was previously well.
Symptoms included cough, exertional dyspnea, constipation (small bowel movements every 2-3 days), abdominal bloating, and frequent burping. Pain assessment revealed constant right-sided dull aching chest pain, intensity 4-5/10, and generalized intermittent, crampy abdominal pain, intensity 5/10.
Medications included hydromorphone syrup 0.3mg p.o. q.i.d., docusate sodium, lactulose, ramipril, folic acid, and salbutamol inhaler.
Findings
Examination revealed decreased right chest expansion with dullness and reduced air entry over the entire right lung field, tympanic abdomen with marked distention, and increased bowel sounds. Neurological exam was normal. There was a large right axillary node. There were cutaneous metastases on the right chest. Body weight was 72kg. Blood urea was 10.7 mmol/L and creatinine was 130 umol/L.
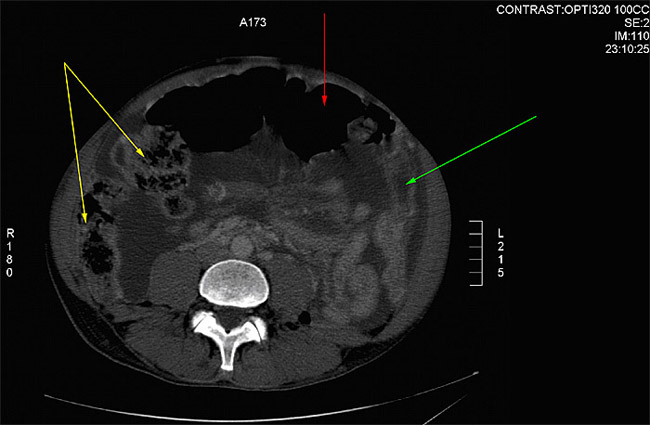
Abdominal CT showed ascites and peritoneal metastases, with compression of the colon in the region of the splenic flexure and proximal dilatation (Fig. 1A).
Figure 1A – dilated transverse colon, full of air (red arrow), hepatic flexure and right colon backed up with stool (yellow arrows), collapsed left colon after splenic flexure (green arrow)
Our assessment of the clinical condition was of incomplete large bowel obstruction, and mild renal failure.
Treatment
The patient was started on DCA 14mg/kg/day (500mg p.o. b.i.d.), supplemented with vitamin B1 300mg p.o. t.i.d. to prevent peripheral neuropathy. He was also started on pantoprazole 40mg p.o. q.d. to prevent GI upset. There was no improvement in pain, or abdominal distension. The patient remained constipated and developed intermittent vomiting. High enemas and increased oral laxative were ineffective. Gastroenterology was consulted regarding insertion of a bowel stent, but they felt the risk of bowel perforation would be high.
After 10 days, we felt there was no benefit so the DCA was increased to 21mg/kg/d (500mg p.o. t.i.d.). Hydromorphone PCA (patient controlled analgesia) was started for pain control at 0.2mg/hr s.c. with patient-controlled bolus does.
After 1 week of DCA at 21mg/kg/d, the patient remained nauseated, constipated, and also developed bilateral leg edema. Abdominal distention persisted. Albumin was 24 g/L, creatinine remained high at 135 umol/L, urea at 10.7 mmol/L. The disease was felt to be worsening and there were no DCA side effects, so the DCA was increased to 42mg/kg/d (1000mg p.o. t.i.d.) in a final attempt to halt tumour progression.
Within 3 days of this increase, there was a marked improvement in appetite and energy level. By 5 days following the dose increase, there was marked reduction in abdominal distention and pain. Several large bowel movements occurred for the fist time in weeks, and leg swelling resolved. The pain level decreased to the point that the patient experienced a relative overdose of hydromorphone, so the infusion was stopped. Renal function was normalized (urea 6.0, creatinine 101).
DCA was then stopped due to development of confusion, agitation and tremors. These side effects resolved within 4 days. After 20 days off DCA, there was clinical evidence of disease progression, and no lingering DCA side effects. A 1 day trial of DCA 500mg p.o. b.i.d. was associated with mild memory problems, so it was stopped. The right axillary tumour was measured to be 3.5 x 5.5 cm.
After another 2 weeks without DCA, the axillary tumour had grown to 4.2 x 6.0cm. At that time, DCA was re-started at 38mg/kg/d with R alpha lipoic acid (to reduce CNS side effects). After 5 days of DCA, the axillary tumour had shrunk to 3.6 x 5.5 cm. DCA had to be stopped again because of mild delirium. It was not restarted.
Then patient’s disease progressed and several weeks later he died due to complications of the cancer.
Comments
This case illustrates one of our earliest experiences with DCA treatment. With our limited experience at that time we felt it was safer to start with a low dose of DCA. Since the condition of the patient was quite advanced, the dose of DCA had to be adjusted quite rapidly and monitored closely. While the lower doses of DCA had almost no effect, a higher dose resulted in quick symptomatic improvement suggesting a response to treatment, and illustrating effectiveness of high dose DCA in a case of mesothelioma. We believe the DCA was responsible for clearing this patient’s bowel obstruction and improving his renal function, since his cancer was constantly progressing prior to DCA and he was not taking any other treatment medications at the time.
DCA also contributed to measurable shrinkage of the axillary tumour. While this showed the effectiveness of DCA, in this particular case it did not have much overall clinical benefit for the patient at his advanced stage.
The side effects were a limiting factor at this higher dose. We noticed side effects of confusion and hallucinations, which resolved in a few days after stopping DCA. We continue to notice these side effects in some of our other patients. They typically resolve within a few days of stopping DCA treatment.
With our experience we now are aware of the benefits of adding R alpha lipoic acid in reducing the CNS side effects. In this case it appears that R alpha lipoic acid was helpful in reducing the DCA-related side effects of confusion/hallucination. It could not however, eliminate the side effects for continued treatment with DCA.