History
A 44 year old male came for consultation regarding treatment of glioblastoma multiforme (brain tumour). He had been diagnosed by MRI 4 months previously when he developed numbness of the left side of his face and left hand. The tumour was located in the right thalamus expanding towards the brainstem and hippocampus. A needle biopsy was obtained, showing grade IV astrocytoma (also called “glioblastoma multiforme”). Due to the location of the tumour deep within the brain, it was considered inoperable. The patient was treated with steroids, 60Gy of radiotherapy and Temodal chemotherapy 140mg daily. There was initial improvement, but the cancer then began to progress again. The patient was offered further chemotherapy with a different Temodal regimen, but he declined due to low success with that drug previously.
Past health problems included depression, non-specific muscle aches and joint pains and prostatitis. Surgical history included appendectomy and recent brain biopsy.
There was a significant history of heart disease in the patient’s family, but no cancer.
The patient smoked for 8 years, but quit 7 years previously. Alcohol consumption was 2-3 standard drinks per week.
Medications at the time of consultation were Oxycontin 20mg p.o. b.i.d. for headache, Lyrica 150mg p.o. b.i.d. for tumour pain, lactulose as needed for constipation, Maxeran 10mg as needed for nausea, and Cipralex for depression. Dexamethasone had been stopped after radiation. The patient had no allergies.
Significant symptoms included intermittent vomiting, intermittent constipation, dizziness, headaches, numbness of the left arm, stiffness of both arms, and a pressure feeling of the posterior neck.
Findings
Examination revealed a healthy-looking male in no distress with normal vital signs and a weight of 69kg. There was mild hyperesthesia of the left side of the body including the left arm and leg. There was also a mild sensory deficit of the left arm, with mild impairment of coordination and mild reduction of power. Cranial nerves were normal. Mental status was normal. Speech was normal. General examination of other systems was normal.
Treatment
The patient wished to have aggressive treatment so we decided to start a combination of DCA and TM. He was started with DCA 29mg/kg/day (1000mg p.o. b.i.d) on a 2 week on / 1 week off cycle. The initial TM dose was 20mg 6 times a day. He was supplemented with zinc acetate 50mg p.o. t.i.d., vitamin B1 100mg p.o. t.i.d., and R+SR alpha lipoic acid 150mg p.o. t.i.d. He was also started on Nexium 20mg p.o. q.d. to prevent GI upset.
The patient was also started back on low dose dexamethasone intermittently (2mg daily only if needed) to control vomiting. Initial ceruloplasmin was 347mg/L, hemoglobin was 135g/L and white cell count was 3.0 (ANC 1.84).
The patient developed some increase in numbness after 2 months of therapy, so the dose was reduced to500mg p.o. t.i.d. (25mg/kg/day) as a precaution. Nerve conduction testing was recommended, but the patient’s specialist did not arrange the test.
Copper deficiency was achieved with TM and zinc. Due to a delay in getting the blood test results, the ceruloplasmin went as low as 60mg/L, and resulted in significant anemia and neutropenia. The patients developed pneumonia requiring hospitalization and i.v. antibiotics. TM treatment was interrupted to allow the white cell count to come back up. Fortunately he quickly recovered as soon as the neutrophil count improved. Ceruloplasmin in the range of 110 to 130mg/L was subsequently maintained with some difficulty (ceruloplasmin target was < 105mg/L but could not be maintained due to recurrent neutropenia).
Zinc acetate was stopped due to copper lowering which was too rapid to allow fine adjustment given the delay in receiving blood results. The patient experienced stabilization of his cancer-related symptoms, and stopped the dexamethasone.
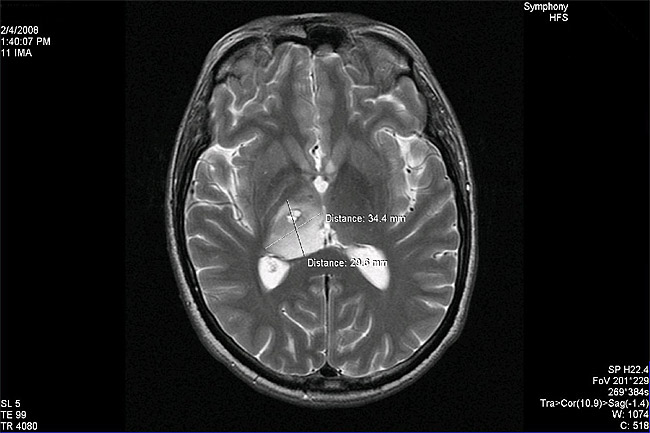
The pre-treatment MRI images were not readily available (the patient was not from Canada) and the translated MRI report did not specify tumour size. After 4 months of DCA/TM treatment a brain MRI was done. The tumour was measured to be 34.4mm x 29.6mm in the largest dimensions:
The patient continued DCA/TM with no serious side effects.
After about 7 months of DCA/TM treatment the tumour had reduced in size to 31.5 x 25.9 mm in the largest dimensions on MRI:
The patient wished to add curcumin at approximately 8 months into treatment. Curcumin 500mg (from A.O.R.) 1 capsule t.i.d. was started.
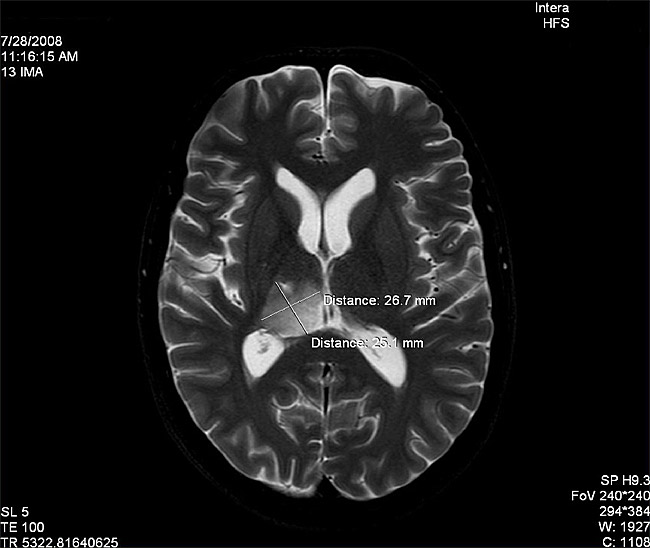
After about 10 months of DCA/TM treatment the tumour had reduced in size to 26.7 x 25.1 mm in the largest dimensions
The patient is presently feeling well, pain is controlled, and he is leading an active life. He experiences occasional bouts of depression. Nerve conduction studies are planned for routine monitoring, and DCA/TM treatment is ongoing.
Comments
This patient represents the longest duration of DCA treatment for our clinic to date (nearly 1 year). We are not clear if this patient developed mild neuropathy, or had a temporary worsening of numbness caused by his cancer. With glioblastoma being one of the most aggressive brain cancers in adults, it is remarkable that this patient is experiencing prolonged and increasing improvement with DCA and TM. The role of angiogenesis inhibiting drugs (like Avastin) in the treatment of glioblastoma is now being recognized. This case supports the principle of using angiogenesis inhibiting treatment for glioblastoma (using TM).
This case also demonstrates the critical role of ongoing monitoring. While these medications are relatively safe, monitoring and adjustment of dosage, side effects and blood tests cannot be over emphasized.
In this case, the tumour was quite big to start with, has not completely regressed but continues to shrink with ongoing DCA treatment. In addition the side effects are mild and tolerable. These findings are in contrast to case 2 above where DCA treatment has been discontinued because majority of the small metastasized tumors have regressed and intolerable side effects. In both this case and case 2, the benefits of TM in tumour stabilization are very encouraging.
This patient has shown us that, once again, it may be possible to transform aggressive cancer from a fatal disease to a chronic disease with simple medications like DCA and/or TM.