History
A 55 year old male attended the clinic seeking treatment for melanoma with brain metastases. It was diagnosed 2 years previously (changing pigmented lesion on the shoulder). This was treated surgically with excision and sentinel node dissection. One of 2 sentinel nodes contained metastatic melanoma. Surgery was followed by standard immunotherapy using interferon alpha for 1 year.
Five months prior to seeing us, the patient developed a solitary left frontal brain metastasis which was treated successfully with stereotactic radiation (Gamma Knife). Just prior to seeing us, the patient was diagnosed with recurrent multiple brain metastases on routine CT scan of the head. MRI 2 weeks prior to seeing us showed 4 brain lesions (see below). CT of the chest also showed over 100 lung lesions. He was offered whole brain radiation, but declined and started Temodal chemotherapy instead. This was stopped prior to completion of 1 cycle due to side effects.
The patient was otherwise healthy aside from hypertension. He was taking some natural supplements including IP6, omega 3,6,9 and Flor-Essence, but no other treatment medications. He had no neurological symptoms.
Findings
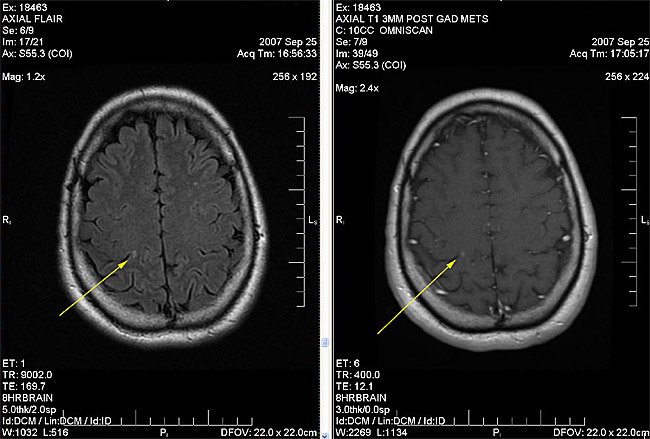
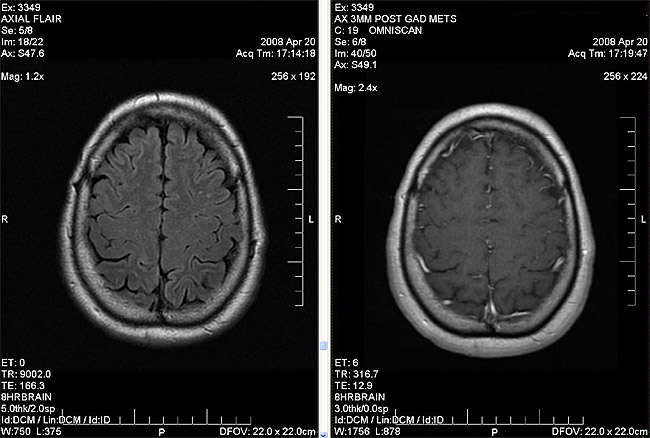
Body weight was 94kg. Physical examination revealed high blood pressure. There were no neurological findings. The rest of the examination was normal. Brain MRI report from 2 weeks previous to the first visit with us revealed 4 small brain metastases (see Fig. 2A)
Figure 2A
Treatment
We elected to try a combination of DCA + TM. The patient was started on DCA 27mg/kg/day (2500mg daily divided b.i.d) on a 2 week on / 1 week off cycle + TM 20mg p.o. six times daily. Pre-treatment ceruloplasmin was 310mg/L, and other blood tests were normal. The patient agreed to follow a copper-reduced diet (no liver or shellfish, copper-free bottled water).
The patient did not have any immediate side effects from DCA or TM. A repeat MRI was planned for 6 weeks into treatment to assess response, but the hospital had a cancellation and moved up the MRI (we were not aware of this otherwise we would have deferred it by about 1 month). It was unchanged, confirming at least 4 brain metastases (Fig. 2B).
Figure 2B
Figure 2C – a right occipital metastasis (arrow)
Figure 2D – left frontal metastasis (top arrow) and a right occipital metatstsis (bottom arrow)
DCA and TM were continued, and copper deficiency in the target range of 20-30% of normal was achieved by 6 weeks with mild neutropenia. TM was adjusted to maintain a ceruloplasmin of 90-100mg/L. The patient was able to maintain normal hemoglobin and a neutrophil count which varied between normal and slightly low using an average TM dose of 20mg t.i.d.
After 3 months of DCA + TM, the patient began to develop some numbness in the toes and fingers bilaterally. We presumed this was early DCA neuropathy. Since the patient was feeling generally well (no other new neurological symptoms to suggest growth of brain tumours), we stopped the DCA as a precaution. Nerve conduction testing was not done at the time as it was not required. TM was continued and copper deficiency was successfully maintained. The only other symptom noted was mild fatigue.
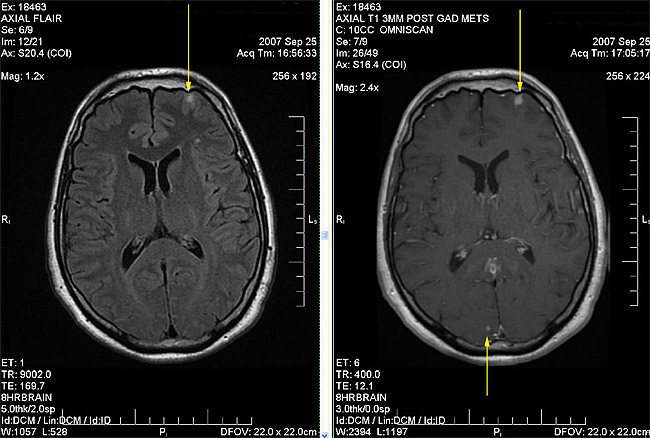
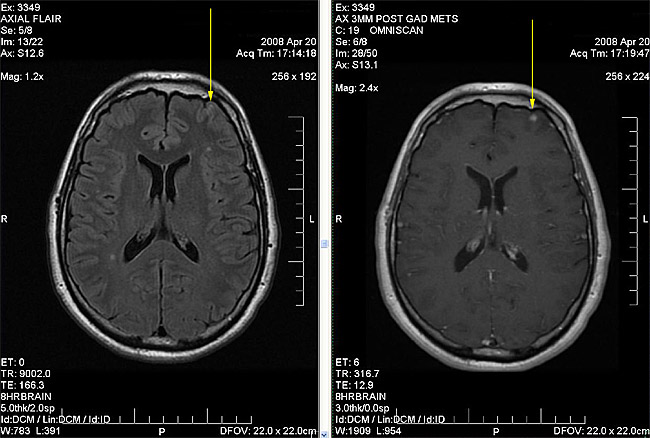
After a further 5 months (total 8 months of TM treatment), brain MRI was repeated. This revealed resolution of all metastases except 1 which was smaller then the previous scan (Fig. 2C). The numbness of the fingers and toes was nearly resolved at that point.
Figure 2E
Figure 2F – right occipital metastasis that was visible on last MRI (see arrow Fig. 2C) is no longer seen
Figure 2G – left frontal metastasis was 7mm on last MRI (Fig. 2D), now 5mm with no surrounding edema
The patient continues to do well on TM alone after a total of 11 months of treatment with no neurological or respiratory symptoms to suggest growth of brain or pulmonary metastases. The patient experiences a moderate amount of fatigue. Follow-up chest CT and brain MRI is planned.
Comments
In this case, we used a combination treatment of DCA and TM. We had experience with both DCA and TM separately and chose to combine them to optimal benefit. Since both medications are quite safe, work by different mechanisms (which could enhance the effect of each other and would likely have no interaction) and have been shown to be effective in other types of cancers, it was felt to be a good choice for this patient. The patient decided to try this combination after a detailed discussion of the various aspects of treatment.
This case illustrates an excellent response of melanoma to a combination of DCA and TM. In the absence of other active treatment, it appears that DCA contributed to the tumour shrinkage as evidenced by the post-treatment scans. DCA treatment was stopped because of side effects. Since TM was being given concurrently and seemed to be having the desirable effect of tumour stabilization, DCA was not restarted.
This case also illustrates the potential for “long-term” benefits of TM (approaching 1 year in this case, with no sign of deterioration). It may be possible to transform metastatic cancer from a fatal disease to a chronic disease with this medication, provided the body continues to tolerate long-term copper deficiency. One theory is that cancer which responds well to TM cannot become resistant since one of the raw materials essential for growth (copper) is deficient. This is different from standard receptor-blocking angiogenesis inhibitors which cancers eventually become resistant to.
We believe that DCA and TM in contributed to tumour shrinkage and tumour stabilization respectively in this case. Once DCA was stopped due to side effects, TM continued to stabilize the tumour potentially eliminating the need for continued DCA treatment. As long as the patients’ condition remains unchanged, we plan to continue this regimen with ongoing monitoring.